Although 10% of those over 60 develop a vision-impairing disease called Age-Related Macular Degeneration (AMD), 66% of participants in a recent survey of 8,000 people from Argentina, Brazil, Colombia and Mexico said not knowing the disease. In parallel, 76% of those consulted stated that they did not know what diabetic retinopathy was, a very common condition in people with diabetes 1 and 2, which can also lead to macular edema.
They are two paths that lead almost to the same place: an undesirable clinical condition that can cause irreversible damage to sight and even cause blindness. In the first case, the problem is related to aging, no small issue, considering that we live longer and tend to have fewer children, which translates into an aging of the population that brings with it this type of problems.
In the second case, macular degeneration is linked to diabetes, a condition on the rise and one of the main “chronic non-communicable diseases”, as the set of non-contagious conditions is called that, such as hypertension or heart disease, are considered a sign of the lifestyle of these times. An important fact is added and that is that type 2 diabetes (90% of cases) has a specific weight in contexts of poverty, since it is closely linked to poor diet.
Data from the WHO recall that the 108 million people with diabetes in 1980 multiplied in 2014 and reached 422 million. According to the International Diabetes Federation, today there are 540 million people with this disease and it is expected that in 2045 there will be 783 million.
Translated, one in eight adults could be exposed to one of the most common consequences in these patients, which is diabetic retinopathy, which in its worsened form can generate macular edema.
 Diabetic maculopathy can be detected in routine ophthalmological check-ups. Photo: Shutterstock
Diabetic maculopathy can be detected in routine ophthalmological check-ups. Photo: ShutterstockWhat is macular edema and why should it be controlled?
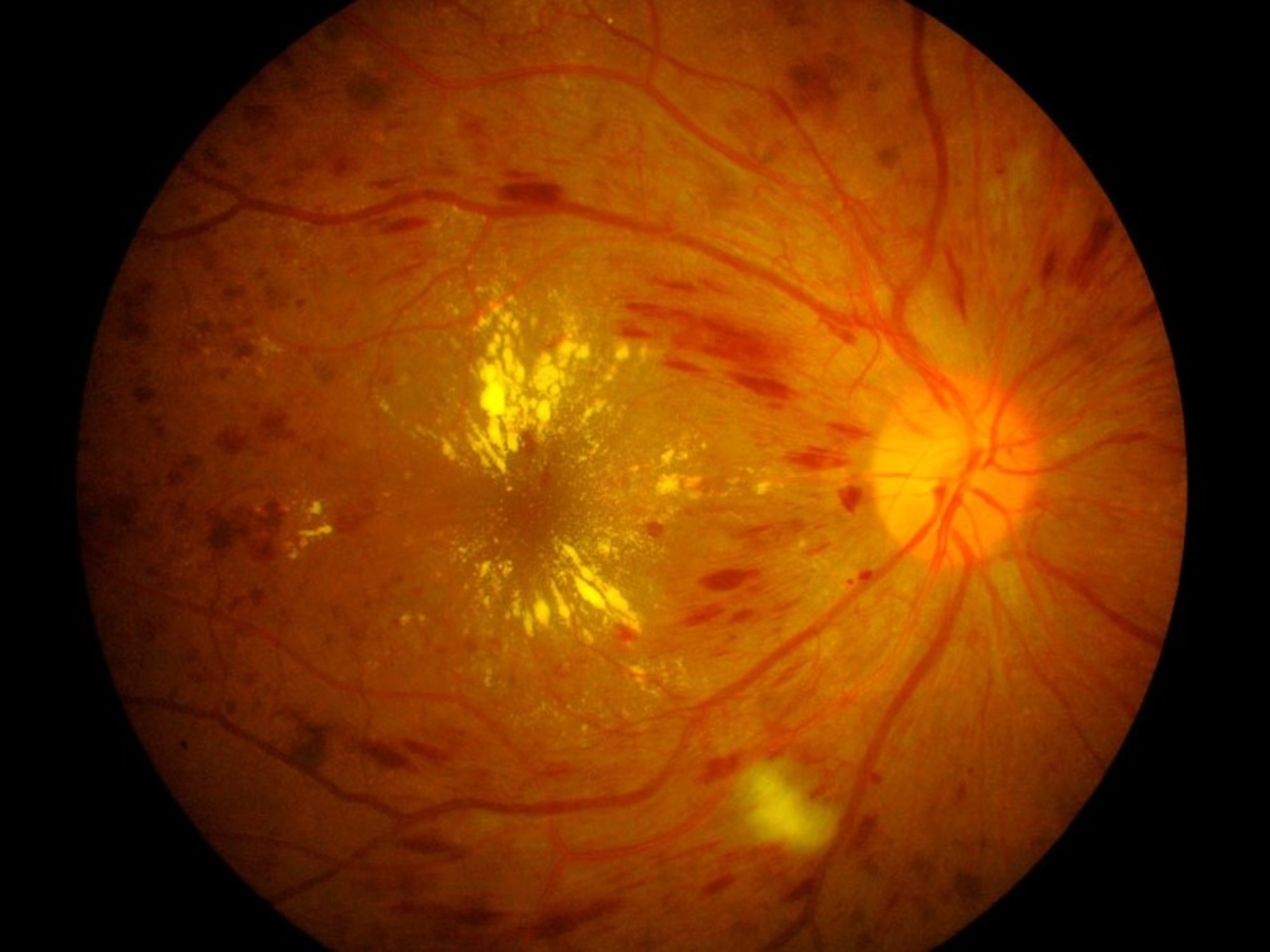
The concept “macular edema” refers to damage or thickening that occurs in a type of light-sensitive film on the back of the retina.
Damage to this film – the macula – can occur both due to the passage of time and due to the dysfunctions caused by the accumulation of sugar in the vessels as a result of diabetes. In both cases, the disease could begin asymptomaticallybut it is detectable with the usual ophthalmological controls.
If perceived, the patient could have distortions in shapes and colors, especially the appearance of black spots in frontal vision and the sensation that straight lines are wavy or deformed, just as when one opens one’s eyes underwater. .
Yes ok there are treatments (and some news that will be discussed at the end of these lines), there is consensus regarding the importance of early detection, precisely to stop the deterioration and recover, to some extent, the lost skills.
Empowered patients against macular edema
The study that reported the population’s lack of knowledge on the subject was carried out by a Brazilian market research consultancy called Ipec (at the request of the multinational Bayer, which markets one of the drugs for the treatment of edema). They participated 2,000 people from each of the four countries mentioned, including 300 with diabetes, in each case.
That Age-Related Macular Degenation (AMD) has been a concept ignored by the 66% of those interviewed It is worrying because of what the prevalence indicates.
 Control of blood glucose level, essential for the treatment of diabetes.
Control of blood glucose level, essential for the treatment of diabetes. Although it is usually said that the disease affects 10% of those over 60% (and reaches 30% in those over 85), the paper Age-Related Macular Degeneration: Epidemiology, Pathophysiology, Diagnosis, and Treatmentpublished in a journal from the Nature group, in 2022, states that AMD affects one in eight adults over 60 and that it is one of the major causes of irreversible blindness in older adults in developing countries
Regarding diabetes, a surprising fact from the study is that while 57% of those consulted considered that the lack of controls for this disease is one of the main causes of blindness (that is, the bridge between blindness and diabetes is present) , 51% of those interviewed considered – strangely – that vision loss is caused by “an infection”, something that could only occur in remote cases.
However, perhaps this other data is more worrying: among the participants who declared themselves diabetic, only 44% said they had received guidance regarding their eye health and referred to consultation with an ophthalmologist.
Dry or wet, how macular edema is treated
The way to treat edema in the macula is related to the form of the condition, which can appear “dry” or “wet.” The first can lead to the second, considered a worsening of the condition.
As in both cases there is a proliferation of inflamed vessels, one of the options, if there is no liquid filtration, is the use of laser, to seal at different points. However, when the picture is wet, the general tendency (what experts call treatment goldstandard) is the use of antiangiogenic drugs, which directly aim to stop the generation of new vessels. They are very expensive treatments and, although they require the application of small injections in the eye, the result is considered superior.
In Argentina, these high-cost treatments are in principle covered, as long as there is an appropriate doctor’s indication. This information was confirmed to Clarion from three sources: the IOMA social work, the PAMI and the Ophthalmology area of the Italian Hospital of Buenos Aires.
The Argentine Society of Ophthalmology (SAO) reports that there are two monoclonal antibodies used for wet edema related to diabetes: bevacizumab, which inhibits the so-called “vascular endothelial growth factor” (or VEGF); and the ranibizumabproduced in cells of Escherichia coli by recombinant DNA techniques.
However, about ten years ago there was a third drug called afliberceptwhich is used in the treatment of macular edema, both due to age and diabetes.
The problem of adherence of patients with macular edema
In Argentina, the use of aflibercept 2 milligrams It has been approved since 2015 and in its “Guide for the diagnosis, treatment and complications of diabetic macular edema and diabetic retinopathy” (a “consensus” document published in 2022), the SAO dedicates six pages to this drug with emphatic recommendations based on various recent clinical studies. They claim that this drug, in several senses, offers superior results to the others mentioned.
Recent news that is worth highlighting is that, although one of the big problems with the use of antiangiogenics is adherence and the invasive form of application (in the case of afliberceptl, patients must receive injections every six weeksso that there is a tendency to abandon it), in May the ANMAT approved a new version of afliberceptl (the commercial brand is Eylea and it would be available in the second half of this year) with a 8 mg dosagewhich promises greater spacing of injections.
The phase 3 study that followed patients for two years showed that the injections can be received at least every 16 weeks.
It is a new door to the problem of adherence, but it continues to require – nevertheless – the activation of official campaigns that provide more information to the general population and encourage annual ophthalmological control. In particular, to the most vulnerable populations: low-income people and older adults.