Experts from the Spanish Society of Periodontology (Sepa) and the Spanish Diabetes Society (SED) ask health authorities to assume scientific evidence and address the management of periodontal diseases in people with diabetes as a public health issue. … Specifically, the National Health System is required to expand oral care coverage for people with diabetes, a demand that is supported by a report on the association between diabetes and gum diseases.
Diabetes
Very frequent, increasing and with problems in its detection. The most recent epidemiological data in Spain place the prevalence of diabetes mellitus at a rate of 13.79%, with a high prevalence of unknown diabetes (6%) and with numbers constantly increasing. As reported in the [email protected] study, approximately 1,000 cases of type 2 diabetes are diagnosed every day in Spain (about 365,000/year). These data not only show the worrying expansion of this health problem, but also require measures to effectively prevent it, detect it early and deal with its complications early.. In this sense, the collaboration that the dental consultation can provide is key, due to its privileged position to serve people who, in many cases, do not have continuous contact with the national health system and who, therefore, avoid the possibility to undergo some type of control that helps uncover cases of hidden diabetes.
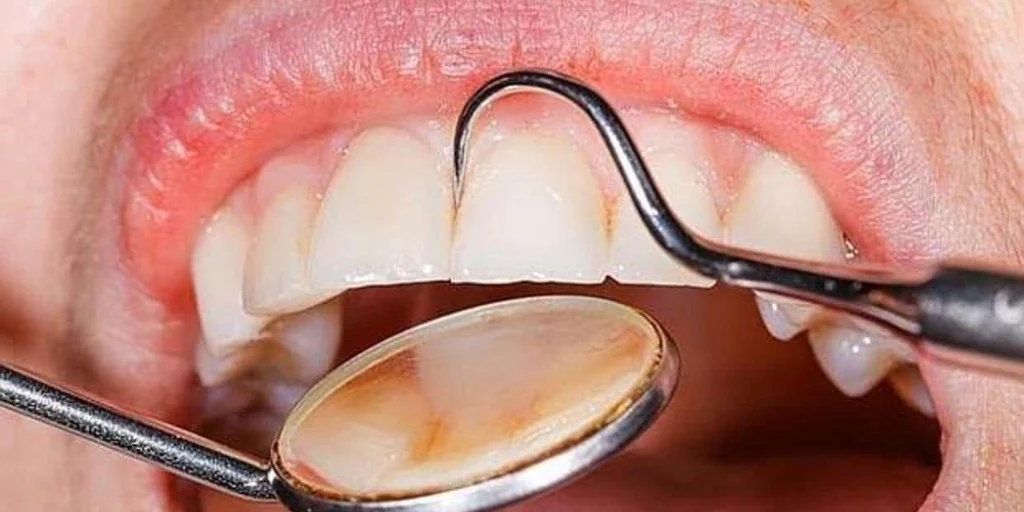
Periodontal diseases
More common than you think and with repercussions beyond the mouth. Periodontal diseases are among the most common non-communicable chronic conditions. For example, a disease such as advanced periodontitis is the sixth most prevalent pathology in the world. The epidemiological data collected in Spain suggest, according to the most complete survey carried out to date, that in adults between 35-44 years old only 14.8% would have healthy gums, 59.8% would have gingivitis, and 25. 4% periodontitis. And in people aged 65-74, only 10.3% would have healthy gums; the rest would present some type of periodontal disease (51.6% gingivitis and 38% periodontitis). Furthermore, the largest oral epidemiological study carried out in Spain on the working population has found 38.4% of people with periodontal treatment needs, this prevalence increasing significantly after the age of 45. The figures are worrying, but even more so if we take into account that diseases such as periodontitis not only have negative repercussions on the oral cavity (tooth loss,…), but its systemic nature places it as a risk factor for developing or aggravating other disorders that threaten general health.
Bidirectional
The high presence of diabetes and periodontal diseases in our environment, which facilitates their coexistence in many people, is not only relevant in itself, but there is also increasing evidence of their close connection, showing it to be a bidirectional relationship.
Risk factor
Periodontitis, a risk factor for suffering from diabetes and for it to appear earlier. In the last 15 years, a series of investigations have emerged identifying periodontitis as a cause of chronic systemic inflammation and as a risk factor for the development of diabetes. An investigation carried out in Spain indicates that patients with advanced periodontitis had an almost 5 times higher risk of developing incident diabetes in a follow-up period between 7 and 9 years. And we must not forget, in addition, that the onset of diabetes at younger ages increases the risk of suffering complications.
Higher risk
Diabetes increases the risk of having periodontitis. Numerous studies have shown that diabetes mellitus (both type 1 and 2) is a risk factor for suffering from periodontitis, increasing the risk approximately three times compared to subjects without diabetes, especially in those with poor glycemic control. The presence of periodontitis makes diabetes management difficult. Periodontitis has been shown to negatively affect glycemic control in people with and without diabetes, and increases the risk of developing kidney and cardiovascular complications. This association is especially relevant in advanced forms of periodontitis.
Periodontal treatment
Periodontal treatment helps control diabetes. Intervention studies carried out in different parts of the world, including Spain, have examined the effect of periodontal treatment on diabetes, highlighting the reduction in levels of glycosylated hemoglobin (HbA1c), one of the most important indicators of metabolic control in diabetes. It has been shown, for example, that people with diabetes undergoing periodontal treatment presented a statistically greater reduction in HbA1c values (0.6%) compared to the control group.
More than a dozen systematic reviews have concluded that there is a significant effect of periodontal treatment on HbA1c levels, a reduction that ranges around 0.4-0.5%. The magnitude of this effect is not negligible in the context of the management of people with diabetes, since each 1% reduction in HbA1c levels is associated with a 35% decrease in microvascular complications associated with diabetes, and a A 0.5% reduction in HbA1c may be comparable to what is sometimes obtained by adding a second hypoglycemic drug.
Headache
Diabetes, a ‘headache’ for the public coffers. A review of studies, including seven of them carried out in Spain, indicated that the total annual cost of a person with diabetes ranges between €1,108 and €6,268, while the strictly health cost is between €687 and €3,643. In addition, it is known that optimal blood glucose control can reduce (up to 30%) the costs of the disease, by reducing the risk of death and the risk of complications. In one of these studies it was indicated that the management of patients with diabetes accounted for 8% of health expenditure, with 5.1 billion in direct costs, 1.5 billion in costs associated with complications and 2.8 billion in loss of work productivity; The annual cost per patient would be 1,660 euros, plus 916 euros for loss of productivity.
Health cost
Impact of periodontal treatment on health costs derived from diabetes. Expanding periodontal care coverage for people with diabetes can mean a significant reduction in the costs allocated to the management of diabetes complications for public coffers. In a study carried out in 2013 by the American medical and dental health insurance company Cigna, the estimated annual savings in those people with diabetes who were adequately treated for their periodontal problems was $1,292 (a 27.6% savings ). Another study has evaluated whether periodontal treatment during the first two years after type 2 diabetes was diagnosed had an impact on costs and utilization of health services in the third and fourth years after diagnosis; Thus, it has been observed that the total health cost in the two years evaluated was 1,799 dollars lower in each patient who had been treated compared to those who had not (the average reduction in health expenditure associated with diabetes was 408 dollars in each patient that period).
Therefore, scientific evidence confirms the importance of periodontal health, especially in people with diabetes. The derived implications have demonstrated the possibility of reducing health costs if periodontal health is improved in people with diabetes, beyond the even more relevant benefits in terms of health and quality of life.
Health authorities must be aware of the scientific evidence and approach the prevention of periodontal diseases as a public health issue. These recommendations also assume that universal access to the public health system must include oral and specifically periodontal diagnosis and treatment, although it is evident that this is not yet the case in Spain.
José Nart. President of Sepa