Late diagnosis is widespread throughout the world, especially in low- and middle-income countries.
|
Highlights -The number of new cases of prostate cancer is projected to increase annually from 1.4 million in 2020 to 2.9 million in 2040. Changes in age structures and improved life expectancy are expected to drive large increases in disease. -The projected increase in prostate cancer cases cannot be prevented by lifestyle changes or public health interventions. -.The only way to mitigate the damage caused by the increasing number of cases is to urgently establish systems for earlier diagnosis in low- and middle-income countries. Screening trials are urgently needed in low- and middle-income countries (LMICs) to better inform ways to improve early diagnosis. -Early diagnosis systems will need to incorporate novel combinations of personnel and integrate the growing power of artificial intelligence to assist in the interpretation of scans and biopsy samples. -As the rise in prostate cancer is likely to be mirrored by the rise in other diseases such as diabetes and heart disease, early diagnosis programs should focus not only on prostate cancer but on men’s health in general. . -Outreach programs that take advantage of the wide global availability of smartphones as tools for prostate cancer education (using both social media and traditional media) are needed, as are programs that help people navigate the healthcare systems. -Most research on prostate cancer has disproportionately focused on men of European descent, even though prostate cancer rates are twice as high in men of African descent. A key research priority is to better understand the factors that influence ethnic differences in disease prevalence. -Treatment of advanced prostate cancer remains an issue and affordable therapies are available, but they are unevenly distributed. Consistent use of these therapies is a cost-effective way to reduce the damage caused by prostate cancer. -There remains a shortage of specialist surgeons and radiotherapy equipment in low- and middle-income countries, and addressing this shortage is key to improving prostate cancer care globally. |
Prostate cancer is the most common cancer by incidence in men in 112 countries (as of 2020) and accounts for one in 14 cancers diagnosed worldwide and 15% of all male cancers.
Among men, the disease is second only to lung cancer in terms of cancer mortality.
Cancers arise in the epithelium that lines the prostate gland: they range from low-grade tumors that do not require treatment to rapidly growing and highly lethal tumors. The disease pathways and some of the underlying biology and genetics are summarized in the Figure 1.
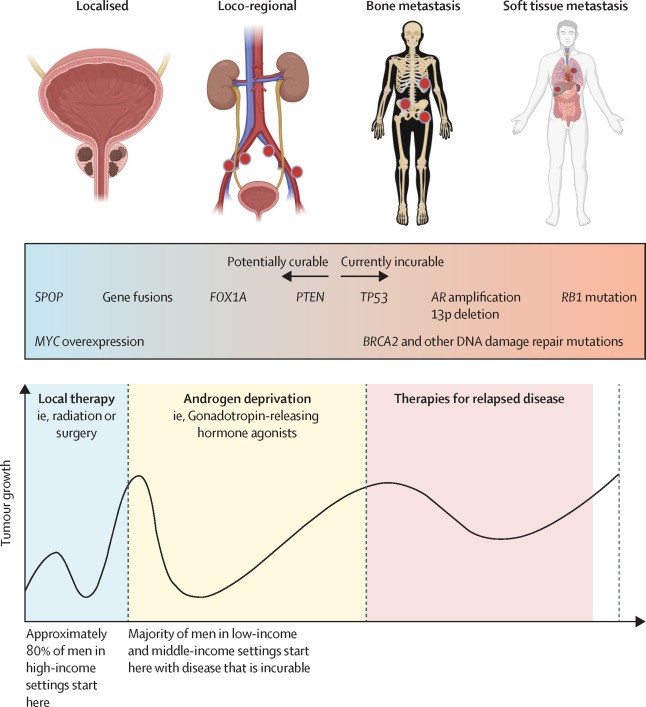
Figure 1. Overview of Prostate Cancer Staging and Biology
The authors projected future trends in prostate cancer cases, identified the best approaches to diagnosis and treatment in different healthcare settings, and recommended evidence-based policies and clinical practices, research, and investments. They sought to empower not only healthcare professionals and providers, but also patients and their families to act as agents of change.
It is likely that advances in imaging (particularly PET and CT with prostate-specific membrane antigen [PSMA]), molecular and genetic technologies, high-precision radiotherapy for curative treatments and new therapies for advanced diseases, together with the use of artificial intelligence (AI) tools, have an increasing role in the detection and treatment of prostate cancer . Many of these technologies are potentially scalable, affordable, and available in low- and middle-income countries, but a major challenge is identifying optimal strategies for their implementation.
The present work is based on key findings from Previous Commissions of Lancet, particularly those regarding access to radiotherapy and surgery. The resulting report of the Commission, which is divided into seven partsprovides an overview of current and future issues and offers recommendations for changes in both policy and practice based on our projections of an increase in prostate cancer cases (primarily in low- and middle-income countries).
| Part 1: Contemporary and future scale and distribution of prostate cancer |
Prostate cancer is already a major cause of morbidity and mortality worldwide, with numbers expected to double by 2040.
The actual number of cases is likely to be higher than the reported figures due to underdiagnosis and poor reporting, particularly in low- and middle-income countries.
Relatively greater aging and population growth in low- and middle-income countries (compared to high-income countries) will lead to even greater increases in prostate cancer in the coming years, causing suffering and economic hardship. The same demographic factors that are driving the increase in prostate cancer incidence will also lead to parallel increases in other diseases in older populations, all of which will need to be addressed by health systems.
With better planning, many of these damages can be substantially mitigated. Solutions with broad applicability are urgently needed. Some possible solutions are discussed later in this Commission, which could include changes in diagnostic and treatment pathways.
| Part 2: The diagnostic route |
In high-income countries, considering opportunistic PSA testing based on informed choices and symptomatic disease presentation for diagnosis results in over-testing in older men and under-testing in younger, high-risk men. However, there are still too many men with advanced disease, especially if they come from disadvantaged socioeconomic backgrounds.
Targeted PSA testing focused on younger men (i.e., 45 to 69 years) in black populations and 50 to 69 years in other populations. Linked to education and outreach programs could reduce overdiagnosis in older men and increase diagnosis in high-risk subgroups of younger men. MRI-based evaluation before referral for biopsy reduces overdiagnosis and overtreatment, while detecting potentially life-threatening diseases.
In low- and middle-income countries, too many men have advanced illnesses, a major social problem that causes suffering, premature death, and financial hardship for families. Furthermore, prostate cancer is just one of a number of diseases, including other cancers, cardiovascular diseases, and type 2 diabetes, that will become substantially more prevalent in low- and middle-income countries in the near future.
Holistic solutions that allow early detection of all these diseases should be prioritized. Prostate cancer awareness plays a central role in effective early detection. To improve prostate cancer diagnosis and treatment globally (especially in low- and middle-income countries) and reduce morbidity and mortality, education is crucial and must be adapted to novel digital approaches.
| Part 3: Management of localized prostate cancer |
The incidence of prostate cancer and other cancers in low- and middle-income countries will continue to increase in the coming decades in line with projected demographic changes, with a corresponding increasing need for facilities and expertise in radiotherapy and surgery. International organizations and commissions should pressure governments to consider both surgery and radiotherapy as priorities in cancer treatment.
Government health coverage should include radiotherapy and surgery to make them affordable for the entire population. Governments also need to fund radiotherapy units and ensure they are sustainable with the help of organizations such as the International Atomic Energy Agency. Each country should invest in at least one comprehensive cancer center that offers radiation therapy and surgery, and should require that center to train local experts. Alternatively, regional centers offer a possible bridge between the lack of provision and comprehensive national services.
The prevalence of prostate cancer and other cancers in low- and middle-income countries will continue to increase as life expectancy increases, with an increasing need for facilities and expertise in radiotherapy and surgery.
In high-income countries, for non-metastatic disease, the emphasis should be on reducing overtreatment in low-risk diseases and reducing the treatment burden in those with higher disease risk (e.g., moving to radiotherapy regimens hypofractionated, avoid excessive use of androgen deprivation therapy). For advanced disease in both high-income and low- and middle-income countries, core therapies must be defined and funded to maximize survival and minimize healthcare costs.
| Part 4: Systemic therapy for advanced disease |