The field of oncology is constantly changing and evolving thanks to rapid advances in research and technology. These advances are leading to new and more effective ways to prevent, diagnose and treat cancer, offering patients a longer life expectancy and a better quality of life. In this sense, the Clínica Universidad de Navarra, together with its Cancer Center and Gilead, have held the “Gilead Chair of Innovation in Oncology” training session.
Throughout this event, a overview of the field of oncologyfrom the current situation in Spain and in the world, through scientific and technological advances and analyzing the emotional and social needs of patients, especially those who suffer from metastatic cancer.
Antonio González, director of the Cancer Center Clínica Universidad de Navarra (CUN) put on the table the data currently being handled about cancer. “Cancer continues and will continue to be a global health problem. 20 million patients with cancer are diagnosed every year around the world and of these, approximately half die, about 9.7 million.” However, despite these figures, the specialist highlighted that the majority of tumors that are diagnosed are preventable. “Lung cancer, which affects a significant percentage of men and women, can be prevented, as can cervical cancer in their case,” he indicated.
The latest data reveal that in 118 countries in the world the The most common tumor in men is the prostateHowever, in the case of the most deadly cancer, the first is lung cancer. On the other hand, in the case of women breast cancer It is the most common in 88 countries, although in some areas, such as the United States and northern Europe, the trend has changed and the first has become lung cancer. Even so, the highest cancer mortality in women continues to be from breast cancer. “Despite this, the good news is that mortality from cancer has been decreasing in recent decades, except for prostate cancer,” González pointed out.
Changes in cancer management

Currently, cancer management is not understood without It is multidisciplinary. As explained by the director of the CUN Cancer Center, “this is what has changed the most in recent years and is what means that each patient receives the best treatment with the greatest probability of curing it. Not only in terms of the multidisciplinary sessions that are carried out to treat any disease and choose the best treatment, but also as part of care, research and training in cancer.”
Another change that has made the approach to this disease different is, precisely, understanding that there are many types of cancer and, furthermore, within each type there is another subtype depending on the mutations and gene expression it presents. This makes oncology has become more complex than it already was and why an oncologist needs the help of other specialists, such as pathologists or psycho-oncologists, so that their patients are treated comprehensively.
Heterogeneous and dynamic tumors
César Rodríguez, president of the Spanish Society of Medical Oncology (SEOM) was in charge of presenting one of the most complex and extensive points of the day: oncological research. “The present approach to cancer is irregular because we are at a time where, depending on the environment in which we operate, the type of tumor and the type of center, we have the perception that in some places this present is more sophisticated and approaches what we call personalized precession medicine. However, in other types of tumors and in other types of scenarios this is still a challenge, although it is really where we are going,” Rodríguez assured.
The specialist insisted that the model that has been followed until now, fundamentally macroscopic, is falling behind because nowadays it is no longer enough to only use imaging techniques that show tumor size or lymph node involvement; They are still important, but not the most. “We have gone from the macroscopic to the microscopic, which would be what was done in pathology services, to give rise to what is molecular oncology,” stressed the president of SEOM.
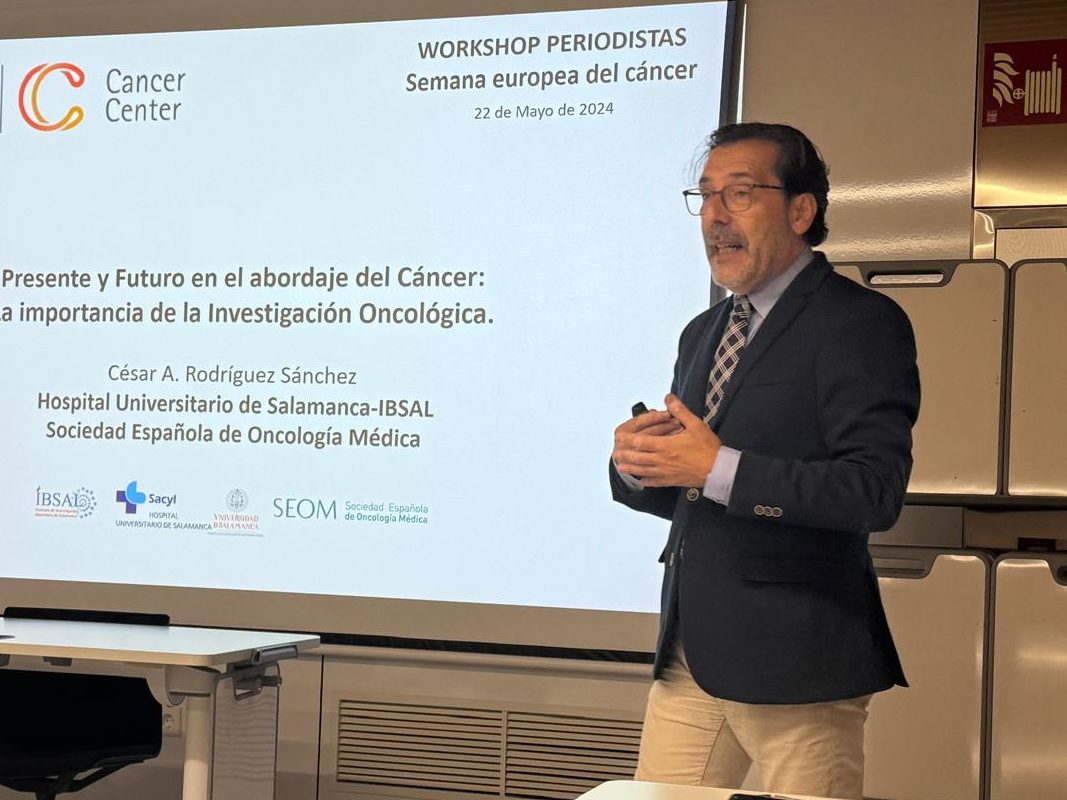
Cancer by definition is a heterogeneous clinical entity, even in the initial stages of tumor development. “If I give you an image of gene expression in different types of breast cancer, you will see that the expression of a luminal breast cancer has nothing to do with a basal-type breast cancer,” said Rodríguez, who added that “Tumors are heterogeneous; there are tumors that are already intrinsically resistant to some treatments, others that will be sensitive and others that are very immunogenic, whose approach will benefit greatly if we stimulate the immune system itself.”
In addition to heterogeneity, cancer is characterized by be dynamic and changing. “As we subject it to therapeutic pressures, we will select resistant clones and this will make the approach more complicated. Those with intrinsic resistance will grow, others will be acquired, etc.,” said Rodríguez, who also pointed out that these changes must be constantly monitored and followed up, something in which the liquid biopsy plays a fundamental role.
Precision medicine
In order to address such a complex disease, it is essential to optimize the greatest amount of knowledge we currently have and make diagnostic and treatment techniques profitable. According to César Rodríguez, “precision medicine is already present in practically all autonomous communities. There are precision medicine plans and we are beginning to implement molecular committees in practically all hospitals or networks. Having as much information about the tumor from the beginning from a genomic point of view is essential. For example, today the treatment of metastatic lung cancer is not conceivable if it is not sequenced.”
This occurs because today a high number of treatable genomic alterations have been identified, that is, they are therapeutic targets that will offer key information for oncologists. These offer prognostic and predictive data, but they also make it easier for professionals to define which treatment will be the best for the patient and which will not provide any benefit. This is very present in lung cancer and, according to Rodríguez, it is beginning to be a reality in breast cancer.
All these advances have led to “going from the peak of escalation and adding treatments to, on the contrary, beginning de-escalation and gradually removing therapies that do not benefit some patients,” said the president of SEOM. In this sense, advances in biomarkers have allowed a change in the treatment of this disease that previously was always treated with chemotherapy and, however, now presents personalized and individualized therapeutic options.
Another technological impact that has improved the oncological approach has been the arrival of artificial intelligence (AI), which allows problems to “obtain and share large amounts of data that allow us to know if it is being done well or not, but also to obtain patients’ perceptions about the treatment they receive and have tools to be in contact with them. It will help us have important real-life data,” Rodríguez highlighted.
In this sense, José María Gutiérrez de Cabiedes, executive director of the CUN Cancer Center, explained the synergies that drive cancer research and highlighted that “Cancer Centers are essential because this disease requires a joint response. Something that already comes from Europe through the plans that he has presented and has in place.”
Information produces hope
On the patients’ side, the event included Pilar Fernández, president of the Spanish Association of Metastatic Breast Cancer, who made a very clear idea: patients need information. “Information does not produce fear, it produces hope,” said Fernández, who also pointed out that not having the necessary information means that patients search for it and do not always find it in truthful places, leading to misinformation.
Pilar also wanted to highlight that the innovations that are being experimented in the oncological field not only prolong the lives of patients, and even cure some, but also improve your quality of life. This is essential in the case of metastatic patients who know that they will not be cured, but with a better quality of life they can live better.
You may also like…