A study published in Science breaks the paradigm that most cases of breast cancer are the result of mutations that occur by chance and accumulate throughout life, which can impact the approach to cancer in the future.
A team of researchers from the Stanford University (United States) has described in a study that the genetics we inherit It influences the surveillance that our defenses make of these mutations, conditioning the type of tumor that can develop and its prognosis. The results, which for the moment refer to breast cancerare published in the magazine Science.
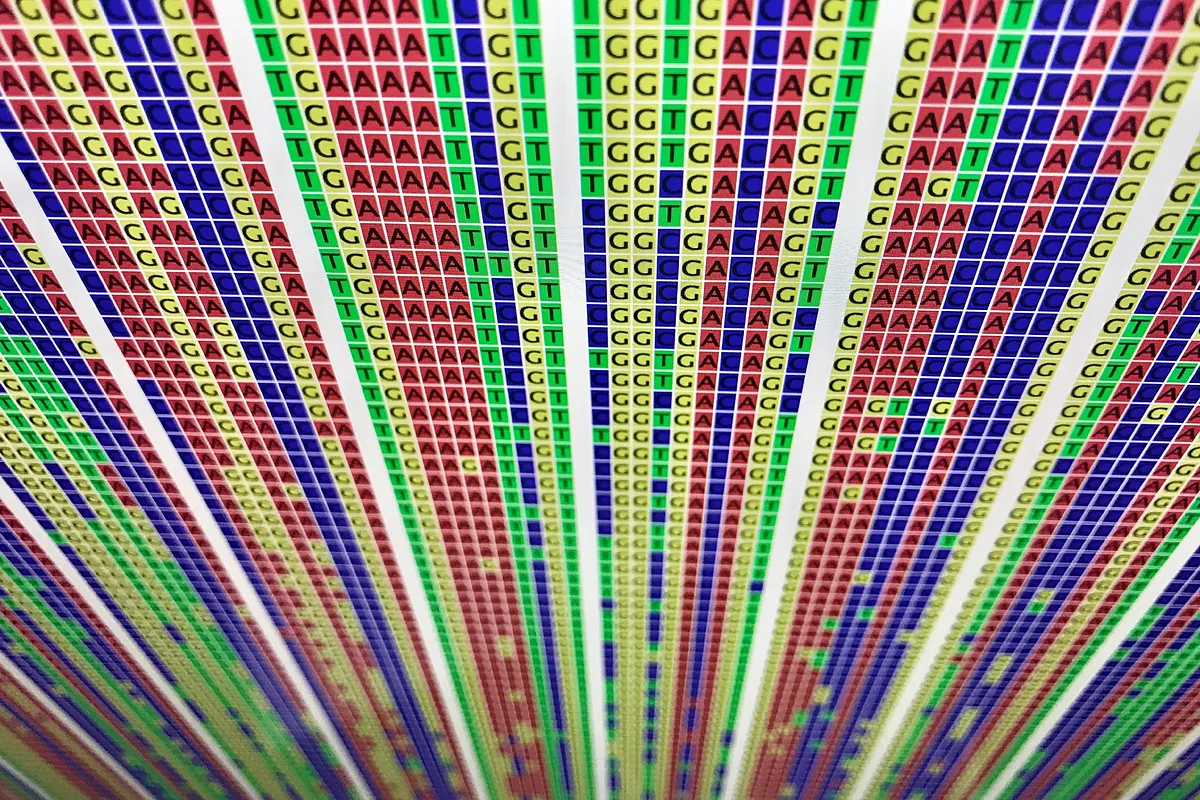
The study, carried out on thousands of breast cancers, has discovered that the genetic sequences that we inherit at the time of conception are powerful predictors of the type of breast cancer we might develop decades later and challenges the dogma that most cancers arise as a result of random mutations that accumulate during our lifetime.
Instead, it points to the active involvement of genetic sequences we inherit from our parents (known as the germline genome) to determine whether cells containing potential cancer-causing mutations are recognized and eliminated by the immune system or passed on. unnoticed to become incipient cancer, explains Stanford University in a statement.
“Apart from a few highly penetrant genes that confer significant cancer risk, the role of hereditary factors is still poorly understood and most malignancies are assumed to be the result of random errors during cell division or bad luck,” he adds Christina Curtis, professor of Medicine and genetics at said center. “This would imply that tumor onset is random, but that is not what we observed.
“Rather, we found that the path to tumor development is limited by hereditary factors and immunity, “which constitutes a new class of biomarkers to predict tumor progression and a completely new way to understand the origins of breast cancer.”
Kathleen Houlahanlead author of the research, points out that “in 2015, we had proposed that some tumors are ‘born to be bad’, meaning that their malignant and even metastatic potential is determined in the early stages of the disease course. Since then, We and others have corroborated this finding in multiple tumors, but These findings shed a whole new light“.
“The study is likely to provide a nuanced and powerful new understanding of the interaction between newborn cancer cells and the immune system, help researchers and doctors better predict and combat breast tumors”.
Currently, only a few genetic mutations are used to predict cancers, but they represent a small minority of cases. These include BRCA1 and BRCA2which occur in approximately one in 500 women and confer an increased risk of breast or ovarian cancerand rarer mutations in the TP53 gene what causes the Li Fraumeni syndromewhich predisposes to tumors.
“The findings suggest that there are dozens or hundreds of additional genetic variants, identifiable in healthy people, that through interactions with the immune system pull the strings that determine why some people remain cancer-free throughout their lives.”
“Our findings not only explain what subtype of breast cancer an individual is likely to develop,” Houlahan said, “but they may also provide clues to how aggressive it may be and its ability to generate metastasis. We believe that these inherited variants may influence a person’s risk of developing breast cancer, something that future studies will have to confirm.
The genes we inherit from our parents are known as germline genomemirrors of the genetic makeup of our parents that give us eye color, hair color or blood group.
Some inherited genes include mutations that confer an increased risk of cancer from the start, such as BRCA1, BRCA2, and TP53. On the contrary, most of the genes associated with cancer are part of what is known as our somatic genome.
Throughout life, our cells divide and die by the tens of millions. Every time a cell’s DNA is copied, errors occur and mutations can accumulate. “DNA from tumors is often compared to germline genomes in an individual’s blood or normal tissues to identify what changes likely led to cancerous transformation of the cell.”
In 2012, Christina Curtis of Stanford University began studying the types of somatic mutations that occur in thousands of breast cancers. He was ultimately able to categorize the disease into 11 subtypes with different prognoses and risks of recurrence, and found that four of the 11 groups were significantly more likely to recur even 10 to 20 years after diagnosis—critical information for doctors making treatment decisions.
Previous studies have shown that people with inherited BRCA1 mutations tend to develop a subtype of breast cancer known as triple negative breast cancer.
“We wanted to understand how inherited DNA could sculpt the evolution of a tumor.” The researchers studied nearly 6,000 breast tumors spanning various stages of the disease to learn whether the subtype of each tumor correlates with the patients’ germline oncogene sequences. The new findings indicate that there are dozens or hundreds of genetic variants additional – identifiable in healthy people – that ‘pull the strings’ that determine why some people remain cancer-free throughout their lives and others do not.
The researchers studied almost 6,000 breast tumors at different stages of the disease to find out whether the subtype of each tumor correlated with the patients’ germline oncogenic sequences.
“We wanted to understand how inherited DNA can sculpt the evolution of a tumor,” he details. Kathleen Houlahan, another of the authors. They found that in the initial, pre-invasive phase, a high load of epitopes – part of a molecule that will be recognized by an antibody – protects against cancer. But once they have been forced to fight the immune system and devise mechanisms to overcome it, tumors with a high load of germline epitopes are more aggressive and prone to metastasis. The pattern is reversed during tumor progression.
It is like a tug of war between the tumor and the immune cells: in the pre-invasive environment, the nascent tumor may initially be more susceptible to immune surveillance and destruction and many tumors are likely to be eliminated in this way and go undetected. “However , “the immune system does not always win” and some tumor cells may not be eliminated.
“Our findings shed light on this opaque process and may shed more light on the optimal timing of therapeutic interventionas well as how to make an immunologically cold tumor warm and more sensitive to therapy.” In the future, the germline genome could be used to further stratify the 11 breast cancer subtypes identified and guide decisions of treatment and improve prognoses and monitoring of relapses.
“The study’s findings may also provide additional clues in the search for personalized cancer immunotherapies and can allow doctors predict a healthy person’s risk of developing invasive breast cancer from a blood test.
The hypothesis that these scientists have demonstrated breaks a paradigm: “that in non-hereditary cancers that appear sporadically (…), the appearance of sporadic mutations and contribution to the creation of a cancer was totally independent of the inherited non-pathological genetic variants. The authors have destroyed this principle“he points out Ramón Salazar, head of Medical Oncology and general director of the Catalan Institute of Oncology (ICO).
“For the first time Inherited genetic makeup has been found to influence immunosurveillance and about the types of somatic or sporadic mutations (not inherited) that can contribute to the appearance of cancer,” continues this expert on the Science Media Center (SMC) platform.
“Some of the hundreds of physiological genetic variants that can occur in a gene determine that the protein they encode (the small chopped peptides that make it up, or antigens) can be presented in a more or less conspicuous manner to the immune surveillance system (T lymphocytes). ) through the antigen presentation receptors on the cell membrane (major histocompatibility system or HLA)”, he details.
The genetic composition of this system is also very variable and can condition that more or fewer copies of the antigens or epitopes, the products of these genes, are presented better or worse, which when they generate cancer are the so-called oncogenes: a gene that has undergone a mutation and has the potential to cause cancer. “When they occur a lot and very well, it is more unlikely that cancer will develop secondary to that oncogene.”
At the moment the study has only been validated for breast cancer and with a type of mutations based on increasing the number of copies of some oncogenes, such as HER2 or MYC, associating the changes with the different molecular subtypes of breast cancer and are being attempted. reproduce it in other tumors and with other mutations.
Science DOI: 10.1126/science.adh8697