False work stoppages, fictitious acts, 100% health… Faced with fraud, Health Insurance is working hard
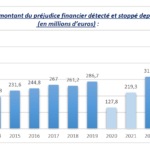


2.4 billion euros by the end of 2027. This is the objective set for Health Insurance by the Attal Government in the fight against fraud. While 2023 was already a “record year”, reflecting “a change of scale” since the end of the Covid crisis, with nearly 466 million euros of fraud and wrongful activities* detected and stopped (+47.7% per compared to 2022), the Cnam will have to go even further, and hit even harder, to reach 700 million euros in 2027.
Because if fraud is the work of a “minority” of policyholders and health professionals, as Cnam executives reminded us three times this Thursday morning, it weighs heavily on public finances. “We repay 250 billion euros each year, a few percent automatically represents a high sum”, underlined Thomas Fatôme. Deviating from the political debate of social fraud “massive” or not, increasing or not, the director of the Cnam has been working since his appointment to “quantify and qualify fraud” to Health Insurance, position by position, profession by profession. Several evaluations have already been carried out (here on general practitioners, and there on other specialists) and will be updated during the year, promises Thomas Fatôme. “What is certain is that fraud is moving to new positions.” And to quote: 100% health, false work stoppages obtained on social networks or even health center fraud…
Pharmacists in the lead
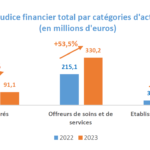
In fact, as Prime Minister Gabriel Attal pointed out last week in his assessment of the plan to combat tax and social fraud, Thomas Fatôme recalled that health professionals (in particular liberals) and others “care and service providers” represent more than 70% of the amount of fraud detected in 2023, compared to 19.5% for policyholders. In terms of volume, the relationships are reversed: healthcare professionals are responsible in 25.9% of cases, compared to 54% for the more numerous insured persons. As for establishments, they generate 9.7% of the financial damage linked to fraud: a figure to be taken with a grain of salt since controls on activity pricing, suspended during the Covid crisis, have not yet resumed in hospitals.
At the top of the most implicated health professionals, we still find pharmacists, for whom the Cnam has detected 60 million euros of fraud in 2023. An amount down sharply compared to 2022 (100 million) which is explained by the “reflux” of cases linked to Covid. Last year, fraud in antigen tests or vaccination nevertheless represented damage of 40 million euros.
With 23 million and 18 million euros of fraud detected respectively, specialists and general practitioners are far behind. But for the latter, the amount of financial damage is up 260%.
On the second step of the podium, health centers are now ranked, which Health Insurance monitors closely because their activity is growing strongly. The 2,500 establishments currently spread across the territory are now reimbursed for 1.4 billion euros, compared to 500 million in 2009. More than 200 checks have been carried out since 2021 – “intense checks, on documents and on site”, underlines Thomas Fatôme. The phenomenon of fraud, “still marginal in 2022”reached a financial loss of 58.1 million euros in 2023, an increase of almost “1000%”. Some networks, through “atypical” noted in their billing but also by the reports received from patients and even employees in several departments, justified the implementation of “task forces” and actions “punch”. “At the start of 2023, we notably launched a simultaneous operation in 9 CPAMs, on 10 sites in the same network”, reported Thomas Fatôme. Results: 21 centers deregulated “emergency” last year and others that will be “probably in the coming weeks”, announces the director of Cnam.
The procedure, put in place in 2020 for serious breaches of the agreement resulting in significant damage (more than 30,000 euros), was also initiated 12 times against liberals in 2023: 9 nurses, 1 midwife, 1 speech therapist and 1 masseur-physiotherapist. “These figures for conventional procedures must increase in the coming years”insisted Thomas Fatôme. “The sooner we stop fraud, the less it will cost us and the less complicated it will be to recover the money behind it.”
In addition to conventional procedures, the Cnam is determined to use all “tools” sanctions: financial penalties (25 million euros in penalties pronounced in 2023), criminal actions (+34% of procedures) or even ordinal (94 seizures). “Nine ophthalmological health centers in the same network were the subject of criminal actions between May 2023 and January 2024”, illustrated the director of the Cnam, listing “an accumulation” criminal charges: fraud, use of forgery, false declaration, etc. “Behind all this, we have fictitious acts, professionals who do not have the titles, serial acts which are carried out on the same families even though there is no identified need.”
Canvassing in nursing homes
Other “new phenomenon” on which the Cnam is focusing its attention: hearing aid fraud. The 100% health reform has generated a wave of change. If the annual number of beneficiaries has increased by 72% since 2021, expenses reimbursed by Health Insurance jumping from 100 to 500 million euros, some 1,500 companies have been created over the last two years… not all with the best intentions. Deputy Director of Audit, Finance and the Fight against Fraud, Marc Scholler distinguishes three types of hearing aid fraud, the financial damage of which reached a total of 21.3 million euros in 2023: one “first layer which corresponds to shortcomings, practices deviating from what is expected”, in terms of monitoring in particular; a second layer of“illegal exercise” and “itinerant activities, canvassing people who do not necessarily need it (notably in nursing homes), to generate turnover”; and a third layer, which represents the majority of the financial damage, made up of companies which organize trafficking, sometimes with the complicity of insured persons (who can sell their Social Security numbers) and doctors, who issue prescriptions without ever seeing the patients.
“The first trends for 2024 show us that we do not have an episodic phenomenon here, but something serious, heavy on hearing aids, which justifies deploying across the whole of France the action plan tested by CPAM 93: making phone calls to people to check that they have a prescription and a hearing aid delivery”insisted Thomas Fatôme.
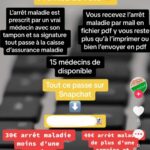
With regard to fraud committed by policyholders, the most numerous, Health Insurance faces both traditional rights fraud (C2S or universal health protection, for example) and identity fraud, and fraud news, facilitated by social networks: false medication prescriptions and false work stoppages (7.7 million euros of fraud detected in 2023)… On the Snapchat network, offers abound: for 15 euros, it is for example possible for us to 'obtain in a few minutes a work stoppage of “2-3 days”, prescribed by a “fake doctor”.
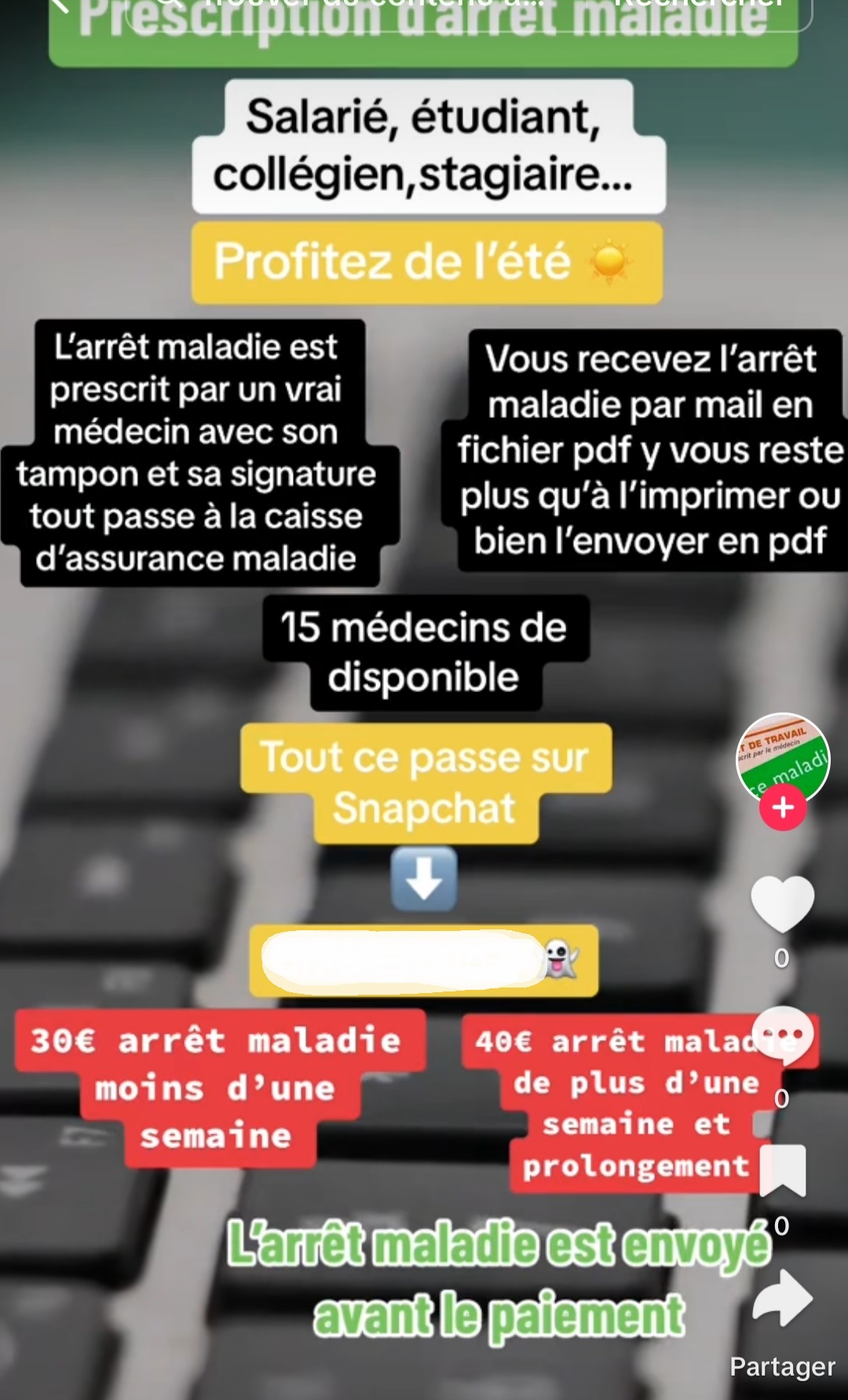
Faced with this new phenomenon, the Cnam is playing the prevention card: after cases of hacking, it has strengthened access to Ameli pro accounts. She also hears “encourage and strengthen“the use of electronic work stoppage, “unfalsifiable”, by doctors. Currently, “more than two thirds” stops are transmitted through this means and it increases by “4 to 5 points per year”; “We are discussing this with the doctors to see how we can further improve things”, underlined Thomas Fatôme. Finally, Health Insurance recruits and trains “cyber investigators”approved and sworn, who have judicial police skills.
*This is activity “abusive”clearly beyond the “need” care, explained Marc Scholler. “The line with fraud is extremely thin.” However, rating errors are not taken into account in these figures.
