The Ministry of Health has given the green light to the financing of a new treatment, based on antibody technology and without associated chemotherapy, for adult patients with follicular lymphoma (FL), an incurable disease. in which relapses are frequentwith results that worsen with each consecutive treatment. ‘Mosunetuzumab’ It is the first and only bispecific antibody approved and financed in our country for these patients, with finite administration and available at the hospitalso these people do not have to wait to start treatment.
In Spain, nearly 2,000 cases of LF4 are diagnosed per year, the most common indolent type (slow growing) non-Hodgkin lymphoma. Despite progress, the disease is still considered incurable. The new treatment from the pharmaceutical company Rocheis indicated for patients with relapsed or refractory follicular lymphoma (not responding to treatment) and who have received at least two prior systemic therapies.
Survival
The therapeutic objective in these patients, as explained by the doctor Juan Manuel Sanchohead of the Hematology Service of the Trias University Hospital i Pujol ICO Badalona (Barcelona) and coordinator of the Indolent Lymphomas Working Group in the Spanish Group of Lymphomas and Bone Marrow Transplants (GELTAMO), “is to increase overall survival with a good quality of life“.
The new treatments, “in addition to being more effective, should have a better toxicity profile compared to conventional ones,” the doctors say.
This, adds the doctor, implies that the new treatments, “in addition to being more effective, should have a better toxicity profile compared to conventional treatments, which have been classically based on cytotoxic chemotherapies.” In this context, he continues, “the availability of ‘mosunetuzumab’ comes to cover a therapeutic need in LFspecifically in those who suffer two or more relapses and who, therefore, have most likely already received chemotherapy regimens in previous treatments“.
Common relapses
This expert also insists that since it is a disease where relapses are common, “the administration of classic treatments based in chemotherapy It leads to cumulative toxicity and, in parallel, a decrease in efficacy, so that the interval between treatments is increasingly shorter with standard therapies.
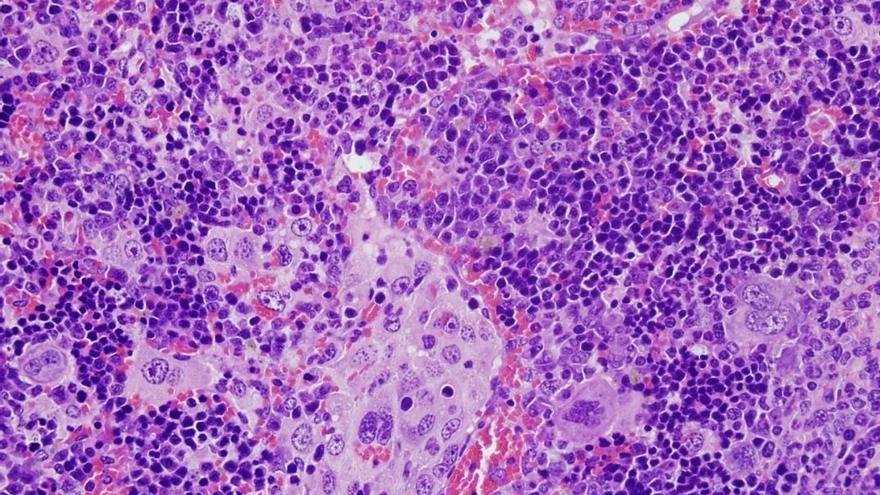
The new option, based on antibody technology and without associated chemotherapy, binds to the patient’s own immune system cells (T lymphocytes)
The new option, based on antibody technology and without associated chemotherapy, binds to the cells of the immune system from the patient himself (T lymphocytes) to redirect them specifically against tumor lymphoid cells. Thus, “the harmful effect is largely avoided that chemotherapy has on healthy cells, while maintaining great antitumor efficacy,” he adds.
Available at the hospital
‘Mosunetuzumab’ is a treatment of finite duration, so patients will be able to reduce their visits to the hospital. For Dr. Sancho, this is one of the advantages, but there are many others such as having a more effective therapy and less toxic regarding the treatments that have been used; which is outpatient, so it does not require hospitalization, and which is immediately available in case a patient requires it.
Add the benefit for the National Health System “having more effective and less toxic therapies means delaying future treatments further. The treatment-free period is extended and by reducing the toxicity of chemotherapy, the healthcare and economic burden that therapies with this type of effects can entail is also reduced. secondary”.
Spanish hospitals
The approval of the new therapy has been based in the positive results of the phase I/II study GO29781, in which four Spanish hospitals (Vall d’Hebron, Barcelona, University Clinic of Navarra, La Paz in Madrid and the Salamanca Clinic).
The study met its primary objective, showing high complete response and objective response rates, 60% and 80% respectively, and a favorable safety profile in heavily pretreated FL patients. The analysis data three-year follow-up showed durable responses maintained over time and a manageable safety profile after treatment, presenting a median progression-free survival of 24 months, Roche reports.