A flat tire and home. Compared to hours spent sitting in a chair at the day hospital for those receiving chemotherapy, patients participating in the clinical trial of what may be the first cancer vaccine can leave in a few minutes.
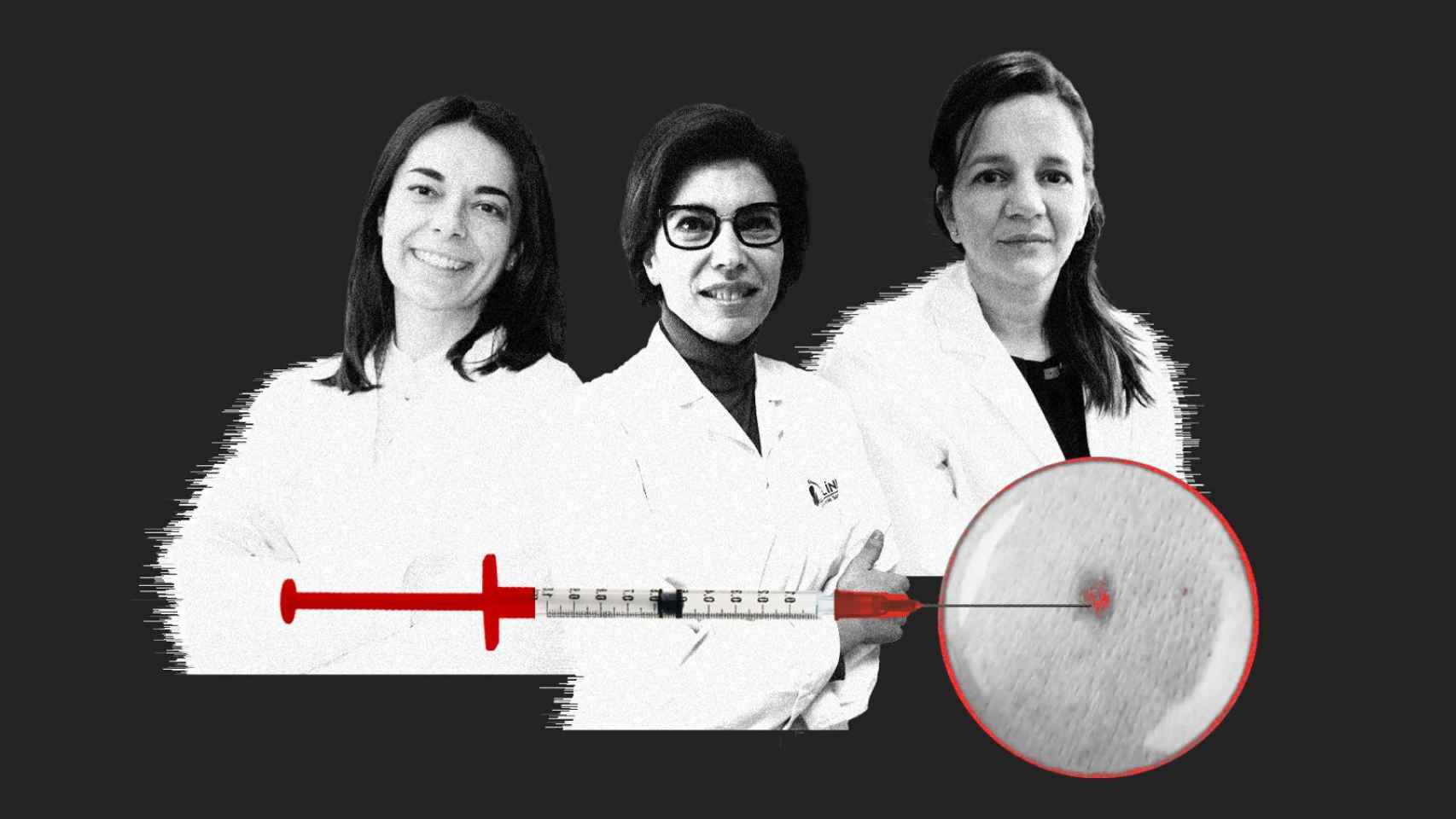
“The first few times we left them under observation for a while, but then they can leave right away,” he says. Eva Muñoz Couseloan oncologist from Vall d’Hebron who is participating in the study.
The only caution is that “it is recommended to rotate limbs.” Each of the nine doses that the patient will receive over the course of a year It will be punctured, alternatively, in one of the two arms or one of the two legs.
In addition, care is taken to ensure that the injection is never in the same arm where immunotherapy is being received, the other treatment that is administered together with the vaccine.
The Vall d’Hebron is one of the five Spanish hospitals where the first cancer vaccine that may come to fruition is being tested.
It is developed by the companies Moderna and MSD and is based on the messenger RNA technology that the first of them launched to immunize us against Covid.
[Adiós al estigma del cáncer: un nuevo fármaco podría evitar la caída del pelo por la quimioterapia]
But it does not prevent cancer: it is a therapeutic vaccine, which seeks to prevent the tumor from progressing again, once surgically removed, in those patients who are at high risk of its reappearance.
The therapy is being tested first in melanoma, a type of cancer that has undergone a revolution in the last decade and a half. It has gone from having few treatment options to two appearing that have changed the course of the disease: immunotherapy first and, if all goes well, this vaccine.
“We already have data from phase 2 of the trial that says that, when receiving the combination of vaccine plus immunotherapy, the death or recurrence rate is 22%, while with immunotherapy alone it is 40%,” explains Muñoz. “That is reduces recurrence by half“.
A round trip to the US
The Vall d’Hebron, along with the other four centers (EL ESPAÑOL has contacted all of them but two have not responded), participates in phase 3, the last one before it can be approved by the regulatory agencies. If these data are confirmed “we will be talking about a new standard of treatment and all tumors in stages IIb to IV would have to be sequenced.”
Because this vaccine, whose provisional name is V940, is completely personalized: it is designed from scratch for each patient. Once this is operated on, a sample of the tumor is sent to the United States, where Moderna has its laboratory.
There the tumor is sequenced and around thirty neo-antigens are obtained, a set of molecules present in the cancer cells of each patient in a unique and exclusive way. The vaccine is manufactured with them and sent to hospitals, where it will be kept at a temperature of -70 degrees. The process takes between three and four weeks.
[El dilema ético de dar quimioterapia 15 días antes de morir: “Cuesta mucho no hacer nada”]
The patient does not wait. “We start with anti-PD1 [la inmunoterapia]which is administered every six weeks, and the vaccine is usually administered with the second dose,” explains the oncologist Ana Arance, who participates in this trial at the Hospital Clínic of Barcelona. “The vaccine is given every three weeks until nine doses are completed. The entire treatment lasts one year.”
The Clinic began to inoculate its first patients at the end of autumn. There are about 15 recruited, coming not only from Barcelona but also from other provinces of Catalonia, although some of them receive a placebo.
It is a common procedure in a clinical trial: each participant is assigned to one of the two arms of the study: the standard treatment (immunotherapy) or the standard plus the vaccine. This will allow the effectiveness of the new treatment to be compared.
In the first group, they are also injected with a placebo. This way, Neither the patient, nor the doctors nor the nurses know who is receiving the vaccine. Thus, his expectations do not influence the results.
In any case, the trial “is randomized to give more weight to the combination than to immunotherapy alone,” explains Arance. More patients receive the experimental treatment than the placebo.
[Jane Healy, vicepresidenta de Oncología de MSD: “La vacuna del cáncer puede llegar antes de lo previsto”]
In Vall d’Hebron they have seven patients in the trial, the first of them started last Christmas. “We received an email from the laboratory, where they explained to us that they were going to do the study and they sent us the protocols and questionnaires to see if we were suitable,” explains Eva Muñoz Couselo.
Normally, the centers that are in charge of clinical trials are usually large and have available and experienced personnel. They also have to serve a sufficient number of patients with the characteristics requested in the trial.
In this case, patients with melanoma that has been surgically removed but are at high risk of tumor recurrencealthough in phase 3 it has been expanded to include patients with a somewhat lower risk.
[Cuando el diagnóstico de cáncer llega antes de los 30: “En lo primero que pensé fue en mis padres”]
“You have to sit down with the patient and explain it well,” says the oncologist. “There are some who don’t quite see it, who don’t feel comfortable with a drug that is not approved. That is why you have to explain very well that it is a safe and already tested drug.”
But, Muñoz continues, “this is not a mortgage: The patient signs a consent form but has the right to leave the trial whenever he wants and without giving any explanation.“.
Once the patient signs their participation, blood tests and imaging tests are performed to control all parameters. A computer program will assign you to one or the other study arm.
A card for each patient
From there, everything will be similar to standard cancer care. Like any other patient, the participants in the trial go to the day hospital: they have seats set aside for them but they are exactly the same as the rest.
There is one thing that does differentiate them from the others. “We give them a card that they must always carry with them so that everyone knows that they are participating in a clinical trial.”
The doctor explains that this is useful if you go to the family doctor or emergency room and they ask about your treatment. “So that non-regular staff know what they are taking and can contact us.”
Melanoma is not the only target of V940. The platform that Moderna and MSD have launched can be applied to anything, although it is known that some cancers are more susceptible to energy boosts from the immune system.
At the Quirónsalud University Hospital in Madrid they are testing this vaccine for melanoma and now they have begun to do it for lung cancer, being the only center in Spain that does it.
[Del cáncer al alzhéimer: así son los “misiles” que están revolucionando la medicina del siglo XXI]
The process is identical, with one exception: after the operation, chemotherapy is indicated, “so first we give them chemotherapy and then they enter the trial,” he explains. Belén Rubio Viqueirahead of research at the hospital’s Oncology service.
Dr. Rubio prefers not to say how many patients are part of the trial at her hospital. Worldwide, it is estimated that 1,089 are included for melanoma and 868 for lung cancer.
V940 is also in late-stage trials in cutaneous squamous cell carcinoma and in mid-stage trials for bladder tumors and renal cell carcinoma.
The main advantage of this new therapy, the oncologist hopes, is “being able to increase survival in exchange for minimal toxicity. “That relapse is delayed as much as possible but also that the quality of life increases.”
Chemotherapy, sometimes maligned, is a treatment with more than proven effectiveness but usually carries a high burden of side effects, such as fatigue, nausea or hair loss.
[El tabú del dolor en el cáncer: así se tratan los tumores que causan más daño a los pacientes]
The new targeted treatments that appeared three decades ago reached areas where chemotherapy had fallen short and significantly reduced adverse reactions. Vaccines would have even fewer unwanted effects than these.
“We have seen that it does not imply added toxicity,” says Rubio. “The only side effect is pain at the injection site, low-grade fever… Like any other vaccine.”
Muñoz also shares the optimism. “The data we already have from phase 2 are provocative and promising.” Ana Arance joins them, pointing out that there is “great expectations with these studies and this type of molecules“.
We still have to wait. The study will last for one year and then there will be long-term follow-up. Preliminary data will come out sooner but Moderna expects it to be completed by the end of the decade. The road to cancer vaccines is long but it has already begun.