



An article by Dr. María Dolores de las Peñas Cabrera,
associate head of radiation oncology at the Rey Juan Carlos University Hospital, Móstoles (Madrid)
vocal for the patient platform of the Oncogeriatrics Group of the Spanish Society of Radiation Oncology (SEOR)
The World Health Organization (WHO) in 20021 defines the active aging as “the process of optimizing opportunities for health, participation, and security with the goal of achieving the best possible quality of life during the aging process.” It is a concept that includes diverse factors such as biological, psychological and social.
There is no unanimity in this definition. We could say that it is continuing to grow and explore satisfaction with one’s life or subjective well-being. In aging, physical and capacity changes occur over time that can limit independence.
In it active or healthy aging, people try to maintain a perfect balance between the profits and losses they observe. It is a process of continuous adaptation to these changes in health, socioeconomic, and resources. The objective is to create a satisfactory and fulfilling environment with the best possible quality of life.
To achieve this goal, it is essential Take care of your physical, mental and emotional health. It is advisable to take care of your diet, maintain regular physical exercise adapted to your general condition, have adequate oral health, avoid alcohol and tobacco, and adjust the strictly necessary medication. All of these recommendations are included in the “European Code against cancer”.
This active aging favors having a decisive and resilient characterfeeling in a safe environment that provides the necessary resources to promote autonomous decision-making.
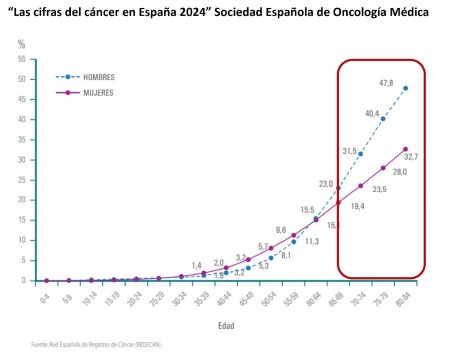
It is known to all that the Increasing age is a risk factor for cancer. Of new cases of cancer, approximately 54% appear in those over 65 years of age and also almost 70% of oncological mortality23 .
The very accelerated pace of population aging in developed countries is going to increase the incidence of cancer. This fact will determine that the approach to older cancer patients is a very serious public health problem. In Spain, according to data from the 2022 National Statistics Institute register, 14.7% of the population, 6,195,588 inhabitants, are ≥ 70 years old.
FIGURE 1. Cancer figures in Spain 2024. SEOM. We observe how this progressive increase occurs after the age of 70.
Therefore, active aging will provide an opportunity for these patients to have the same onco-specific treatment possibilities as younger patients and achieve the same cure rates with a minimum of side effects.
The biological age does not always coincide with physiological or functional age of older patients. Health professionals are aware of this and it has become necessary to search for tools that allow us evaluate custom functional reservation of each cancer patient throughout the natural history of the disease, to adjust the most effective and safe treatment.3
Patients over 70 years of age present characteristics inherent to their age, fragility, vulnerabilities linked to their comorbidities, socioeconomic support limitations, nutritional limitations, sarcopenia, etc.
The Comprehensive Geriatric Assessment (VGI), which Rubenstein suggested in 19894emerges as a «multidimensional interdisciplinary diagnostic process focused on determining the medical, psychological and functional capacity of an older person in order to develop a coordinated and integrated plan for long-term treatment and follow-up».
The presence of expert Geriatricians is necessary in carrying out this Comprehensive Geriatric Assessment applied to the cancer patient. What does the implementation of Oncogeriatrics seek in multidisciplinary care teams?:
- Predict possible toxicities linked to oncological treatments, whether surgical, radiotherapy, chemotherapy, etc.
- Ensure that the patient will be able to tolerate the treatment in its entirety and with the fewest number of adverse effects.
- Guarantee adherence to it to achieve the best possible results.
- Maintain quality of life to the maximum.
- Assess the older patient’s ability to understand their process and participate in shared decision making.
- Resolve doubts about the impact of oncological diagnosis and treatment on previous baseline status.
This will allow us personalize oncological treatment and avoid overtreatment with the risk of complications such as undertreatment, losing healing opportunities. The objective is to adapt oncological treatment not to chronological age but to functional age.
The International Society of Geriatric Oncology (SIOG) published a consensus of areas to consider in this oncogeriatric evaluation in 2014.5. The main ones would be:
- Functional and social situation: assessing abilities to function in daily life. Degree of independence. Where do you live and with whom? Whether you have family support or not, etc. Presence of socio-affective deficiencies.
- Presence of comorbidities: other diseases that limit treatments.
- Cognitive sphere: presence or absence of dementia and its degree.
- Affective or mood state: depression, sleep disorders, etc.
- Presence of geriatric syndromes: risk of falls, for example.
- Physical situation: identify fragility or hidden vulnerabilities.
- Pharmacological history: adjusting treatments that really add value.
- Assess the degree of sarcopenia or muscle functional reserve.
The Comprehensive Geriatric Assessment allows us Stratify patients into four well-defined groups and suggest recommendations or interventions in the different areas discussed, and even related to oncological treatment. Would6.7:
- *Type I or Robust Patient: It does not present signs of frailty or significant comorbidities and has an acceptable vital prognosis, which is why it would be considered subsidiary to standard treatment.
- *Type II or Prefrail Patient: He presents signs of frailty, but has sufficient functional and biological reserve and estimated vital prognosis to benefit from a prehabilitation intervention that could subsequently make him subsidiary to standard treatment.
- *Type III or Frail Patient: The patient presents signs of fragility, but has functional, biological reserve and estimated vital prognosis to benefit from an intervention, although it is foreseeable that complications may arise from this, so adaptation of the treatment is recommended to minimize side effects.
- *Type IV Patient or Poor prognosis: The patient has significant comorbidity and/or dependencies that limit his life expectancy, so we recommend maintaining conservative treatment of his pathology, prioritizing palliative measures in case the patient presents poor symptom control.
FIGURE 2. Classification and treatment recommendations according to Comprehensive Geriatric Assessment. Taken from Rodríguez Couso, M. Nutr Hosp 2020;37(Extra No. 1):38-47.
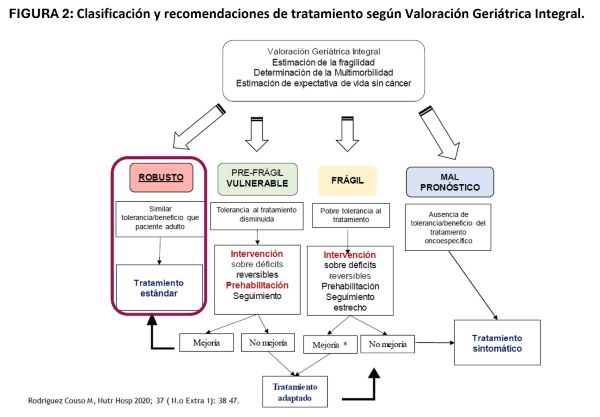
Active aging would make it easier for the cancer patient to be in type I or Robust and type II or Prefragile, optimizing their chances of receiving a effective treatment with minimal risk of effects derived from oncological treatments. They would even be patients in whom if they present vulnerabilities, they can be improved with prehabilitation in the areas that need it.
We must make it easier for health policies to implement action plans to promote active agingsince its impact on the treatment of all diseases is clear and also on the cancer treatment.
Bibliography:
1- World Health Organization. World report on aging and health [Internet]. USA; 2015. p.1–253. https://iris.who.int/bitstream/handle/10665/186466/9789240694873_eng.pdf?sequence=1
2- Ries EM, Kosary CL, Hankey BF, et al. SEER Cancer Statistics Review: 1975-2000. National Cancer Institute, Bethesda, MD.
3- Surveillance, Epidemiology, and End Results (SEER) Cancer Statistics Review, 1975-2015. http://seer.cancer.gov/archive/csr/1975_2015/ (Accessed on July 31, 2019).
4- Rubenstein LZ, Siu AL, Wieland D. Comprehensive geriatric assessment: Toward understanding its efficacy. Aging (Milano). 1989:87–98.
5- Wildiers H, Heeren P, Puts M, Topinkova E, Janssen-Heijnen MLG, Extermann M, et al. International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients with Cancer. J Clin Oncol. 2014;32:2595–603.
6- Peromingo, FJM, Algar, CO, Monedero, MEB, de Villaumbrosia, CG, de Asua Cruzat, DR, & Martín, RB (2018). Proposal for the development of an oncogeriatrics unit. Times of change: our reality. Spanish Journal of Geriatrics and Gerontology, 53(3), 149-154.
7- Rodríguez Couso M. Geriatric interventions in the elderly with cancer based on comprehensive geriatric assessment. Areas of optimization: what the geriatrician can contribute to the multidisciplinary team. Nutr Hosp 2020;37(Extra No. 1): 38-47.
